Utilization Management Teams
Transform your prior auth process with AI
Autodor pre-processes incoming prior auth requests so your clinicians can focus on complex cases. Get faster decisions and fewer delays without sacrificing accuracy.

APPROVE MORE, DENY LESS
20x your team’s prior auth review capacity with Autodor
Utilization management teams face growing review volume, pressure to reduce turnaround times, and inconsistent application of clinical criteria. With Autodor, seamlessly streamline prior authorization workflows, helping your plan reach new levels of efficiency.
Pre-process prior auth requests
Autodor automatically gathers critical data from clinical records, flags missing information, and delivers a ready-to-review summary—so your clinicians spend less time compiling and more time making informed decisions.
Accelerate care approvals
Handle rising volume with greater speed. With Autodor, common authorizations can be approved within seconds, reducing admin time and increasing access to care.
Support specialty cases
Tackle complex reviews with confidence. Trained on your policies, Autodor understands intricate benefit rules and applies policy-aligned logic to each review.
.gif)
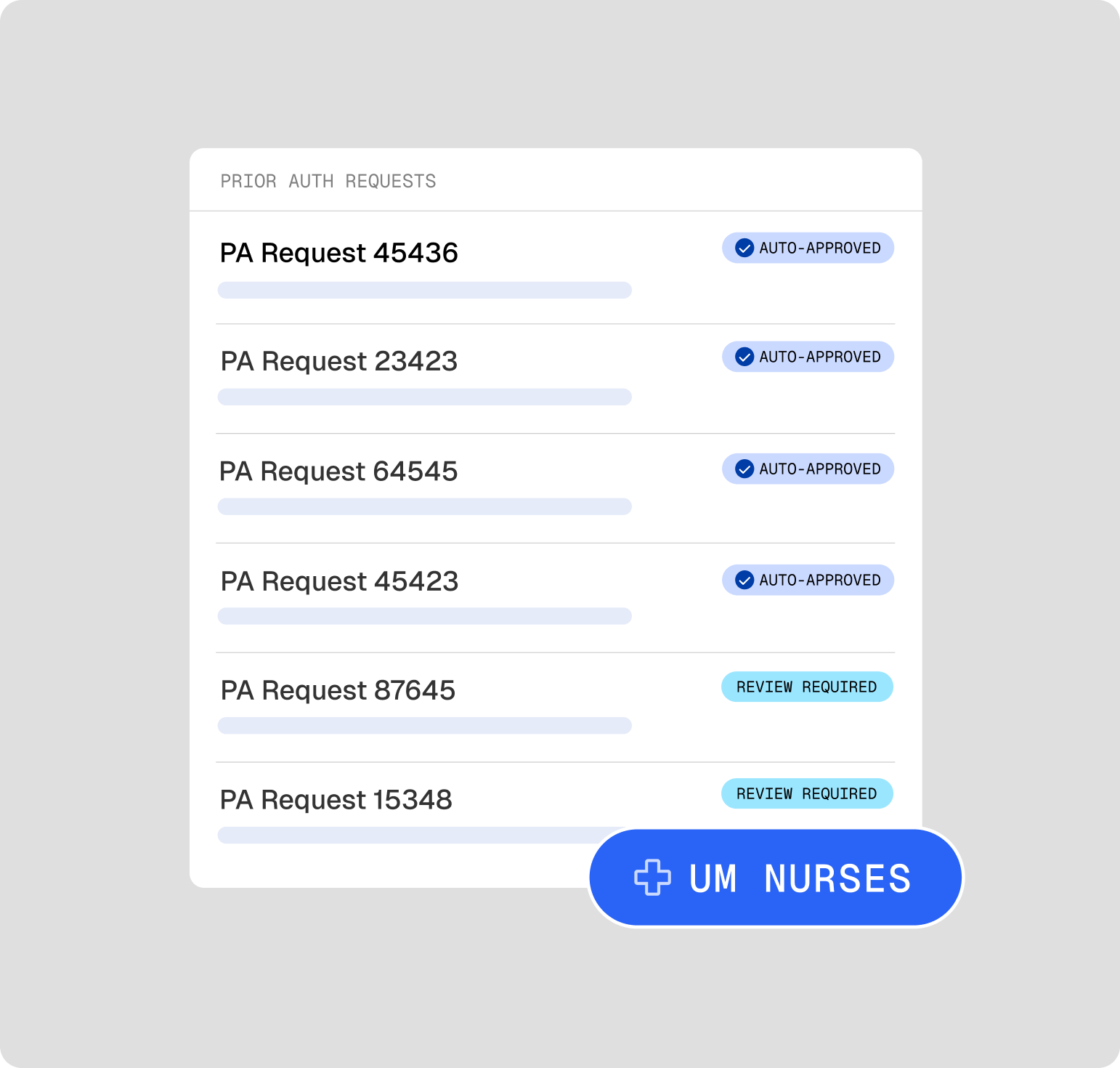
Smart triage, real savings
Autodor intelligently categorizes requests based on risk and required expertise. Straightforward cases are routed to fast-track approval, complex cases are routed to the right clinician.
Intelligent clinical reasoning
Autodor clinically reasons against medical records, policy guidelines, and relevant clinical criteria to provide smart, relevant recommendations.
Human validation
Every AI-generated recommendation comes with evidence and policy citations, making it easy for your team to review, validate, and act quickly.
Power prior auth with Auto Agents
Seamlessly build, manage, and scale your prior authorization process with Auto Agents—trained specifically to meet the complex needs of UM teams.
Prospective, Concurrent, and Retrospective Reviews
Emergency Department Reviews - EMTALA and Prudent Layperson
Level of Care Reviews
High-Cost Drug and Specialty Pharmacy Reviews


One enterprise-level platform for health plans
Alaffia’s all-in-one AI platform pairs clinical expertise with advanced AI to boost clinical productivity, eliminate wasted spending, and streamline admin tasks.
"Alaffia is streamlining how medical claims are processed and reviewed. They're applying AI and machine learning in new ways that will reduce burden and lower costs across the industry, which will free up resources to more equitably care for patients."
Dr. Andrey Ostrovsky, Former CMO, US Medicaid
Frequently asked questions
Implementation timelines can vary based on your specific use case and current systems, but most Alaffia customers go live within 30 days. We take a collaborative approach by starting with an in-depth review of your current workflows before technical integration and workflow configuration.
Yes, Alaffia integrates seamlessly with a wide range of authorization systems, including EHRs, UM platforms, and custom-built tools. We can work within your current ecosystem without requiring disruptive system changes.
Our Autodor platform uses a combination of clinical AI, large language models (LLMs), and policy-based logic to analyze claim data and provide recommendations.
Clinical context is extracted from unstructured notes, attachments, and claims.
Your guidelines or industry standards are encoded and considered.
The AI generates a pre-processed case summary, highlighting clinical facts, missing information, and a recommendation aligned with your plan policies.
Every recommendation is reviewed by a human. Our AI is never used to deny care, and always supports clinician judgment.
Autodor and Auto Agents are highly customizable for your specific health plan’s needs. We train our Auto Agents to reflect your internal guidelines, clinical policies, and documentation requirements. Whether you’re handling oncology prior auth or specialty pharmacy reviews, we configure custom workflows to follow your specific criteria, flag cases, and route complex claims to clinicians.
Drive health plan affordability with Alaffia
Discover how our clinical review platform drives real savings for your plan.


