
Deeper insights. Better outcomes.
Purpose-built for health plans, our AI platform helps claims teams provide truly defensible findings with an extremely low appeals rate. We’ve achieved 97%+ accuracy across all client implementations.





Document digitization
Auto Agents transform PDF files and scanned images of all sizes into actionable data assets.

Smart evaluation
Auto Agents clinically reason against your medical records, policy guidelines, and relevant clinical criteria.

Transparent recommendations
Auto Agents cross-reference documents to provide clear rationales and citations for each claim recommendation.

Streamlined human validation
Clinicians validate the Auto Agent’s responses, ask final questions, and complete the claim.
Custom AI agents for any workflow
Developed with our clinicians, configured for your needs.
Utilization Management Agents
Streamline approval decisions with made-for you AI that applies clinical guidelines consistently across all review types.
Prospective, concurrent, and retrospective reviews
Emergency department reviews - EMTALA and prudent layperson
Level of care reviews
High-cost drug and specialty pharmacy reviews

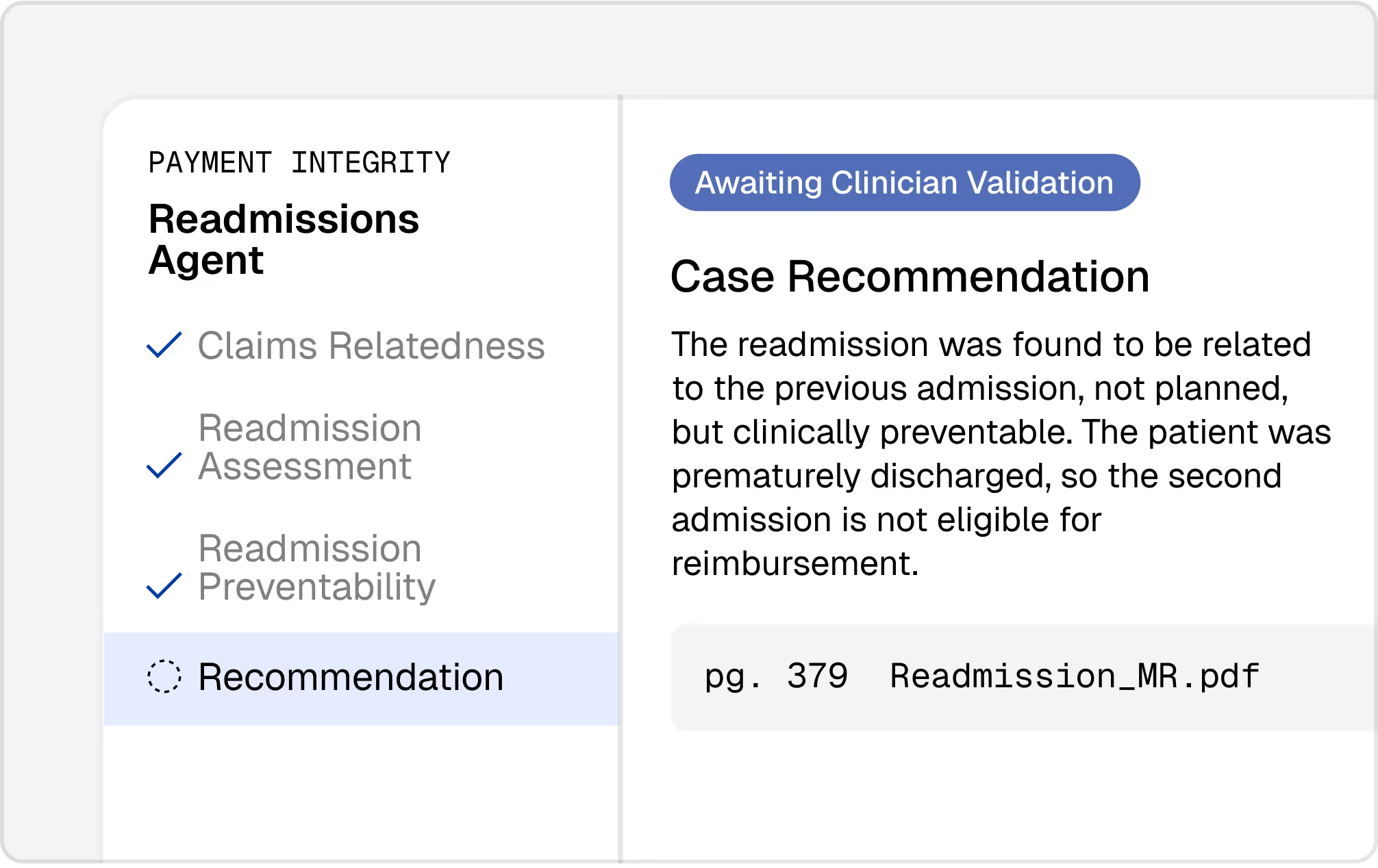
Payment Integrity Agents
Identify clinical validation opportunities and reduce payment errors with an AI agent that thoroughly analyzes documentation against evidence-based standards.
DRG clinical validation (sepsis, cardiovascular conditions, respiratory conditions, and more)
Medical necessity reviews
Readmission reviews
Short Stay Reviews
Appeals Agents
Transform your appeals department with the support of AI to evaluate clinical documentation, apply relevant policies, and draft evidence-backed responses.
Pre- and post-service appeals
Emergency service appeals
Level of care appeals
DRG & coding appeals


Smart triage that lets your clinicians do their most valuable work
Our AI agents review clinical cases 20x faster than human clinicians, routing clear approvals for immediate processing while flagging complex cases. That frees up your clinicians to focus their time and expertise where it matters most.
See how Alaffia's AI can transform your claims operations
AI trust and safety
Privacy, security, and compliance are built into every layer of our solutions. We adhere to SOC-II Type II, HIPAA, and HITRUST security standards to keep member and payer data private and secure.
Human-led validation
Every recommendation includes a clear clinical rationale and traceable source citations, with links back to medical records and policy documents for human verification.
Custom governance controls
To ensure adherence to your organization’s specific data governance requirements, we establish and implement custom governance controls.
Enterprise-grade security
All data stored within our platform is encrypted in transit and at rest, with 256-bit encryption to protect confidentiality and privacy.
Drive health plan affordability with Alaffia
Discover how our clinical review platform drives real savings for your plan.








